laser interstitial thermal therapy
Laser Interstitial Thermal Therapy (LITT), also known as MRI-guided laser ablation or stereotactic laser ablation, is a highly advanced, minimally invasive neurosurgical technique used to treat brain tumors and other neurological lesions.
It offers an alternative to traditional open craniotomy for specific patient populations and tumor types, especially those that are deep-seated or located near critical brain structures.
The Procedure
How LITT Works
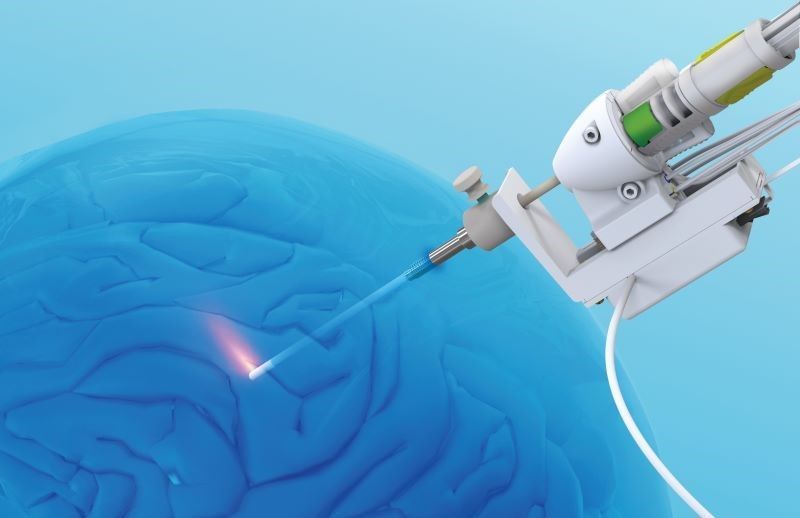
LITT uses focused heat to destroy (ablate) targeted tissue with precision, guided by real-time magnetic resonance imaging (MRI).
- Stereotactic Targeting: The surgeon uses pre-operative MRI and computer-guided navigation to precisely map the tumor's location.
- Minimal Access: While the patient is under general anesthesia, the surgeon makes a tiny incision in the scalp and drills a small hole (about the width of a pencil\approx 5mm) in the skull.
- Laser Placement: A thin, flexible fiber optic laser probe is then inserted through the hole and guided stereotactically to the center of the target tissue (the tumor).
- Thermal Ablation: The laser is activated, transmitting energy that heats the tissue at the tip of the probe. High temperatures (cause rapid, irreversible coagulative necrosis (cell death) in the tumor.
- Real-Time Monitoring: This is the most critical feature. The procedure is performed inside an MRI machine, which generates a live, color-coded thermal map of the patient's brain. This allows the surgeon to: Continually monitor tissue temperatures, ensure the laser damage is contained within the tumor margins, and protect surrounding healthy, "eloquent" (critical function) brain tissue.
Applications for Brain Tumors
LITT is an increasingly accepted treatment option for a variety of brain tumor-related conditions, particularly:
- Recurrent/Progressive Malignant Tumors: Used for high-grade gliomas (like Glioblastoma, or GBM) and brain metastases (cancers that have spread to the brain) that have recurred or progressed after initial treatment (surgery, radiation, or chemotherapy)
- Deep-Seated or Inoperable Lesions: Tumors located in difficult-to-reach or eloquent areas of the brain where open surgery would carry a very high risk of permanent neurological damage
- Radiation Necrosis: Treating symptomatic areas of dead brain tissue that can occur years after radiation therapy, which can often be difficult to distinguish from a recurrent tumor on an MRI.
- Palliative Care: Shrinking tumors to alleviate severe symptoms and improve the patient's quality of life.
- Tumor Size: LITT is generally most effective on smaller lesions, typically less than 3 cm in diameter.
After the Procedure
Advantages and Recovery
LITT's minimally invasive nature provides several significant benefits over traditional open surgery (craniotomy). Benefits:
- Incision Size: Paper-cut sized incision; pencil-width hole in the skull.
- Hospital Stay: Typically 1 night (often discharged the next day).
- Recovery Time: Return to normal activities in 1-2 weeks
- Pain/Scarring: Minimal pain (often managed with over-the-counter medication) and minimal scarring.
- Biopsy Capability: A biopsy can be performed through the same trajectory before ablation to confirm the diagnosis.
Risks
While minimally invasive, LITT still carries risks, though generally lower than open surgery. The main risks include bleeding/hemorrhage, new neurological deficits (e.g., temporary or permanent weakness, vision or speech problems), and swelling (cerebral edema), which is usually controlled with medication.