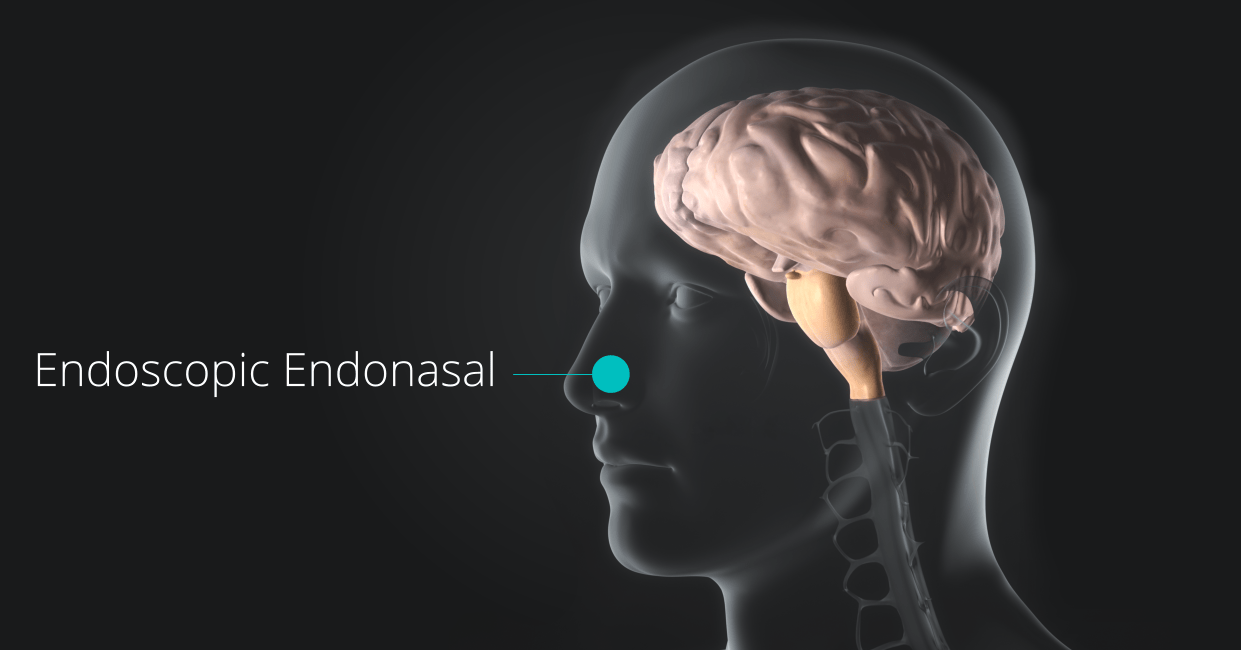
Endoscopic Endonasal approach
Orange County neurosurgeon Robert Louis, MD specializes in minimally invasive endoscopic endonasal and endoscopic transsphenoidal surgery for removal of tumors in the pituitary gland, sellar region, and sphenoid sinus of the skull. Along with his partner, Dr. Tim Kelley, the team at Hoag Memorial Hospital has performed more than 1,000 of these operations successfully over the last decade.
With this sophisticated technique, Dr. Louis approaches the pituitary through the nose using a microscope and a light called endoscope. Pituitary tumors cause a variety of hormone problems and can grow to large size, compressing important nerves and arteries at the base of the brain. When this occurs, surgery is needed to remove the tumor, especially when vision is at risk. This approach is most commonly used for the treatment of pituitary adenomas, Craniopharyngioma, Rathke’s cleft cysts, sinonasal carcinoma, olfactory neuroblastomas, and meningiomas.
The Procedure
Endoscopic Endonasal Pituitary Surgery
This procedure is a type of transsphenoidal surgery, meaning it goes through the sphenoid sinus.
Minimally Invasive: The surgeon accesses the pituitary gland through the nostrils and nasal passages, avoiding the need for an external incision on the face or a craniotomy (opening the skull).
The Endoscope: A thin, rigid tube with a light, camera, and microscope (an endoscope) is inserted through the nose. This provides the surgical team with a clear, magnified view on a monitor.
Team Approach: The surgery is performed jointly by a neurosurgeon and an ear, nose, and throat (ENT) surgeon or skull base surgeon.
This method is considered the "gold standard" for surgically treating most pituitary tumors.
Reasons for the Surgery
The primary reason is to remove tumors of the pituitary gland, called pituitary adenomas, which can be hormone-secreting (causing conditions like Cushing's disease or acromegaly) or non-hormone-secreting.
Common symptoms that lead to this surgery include:
- Vision Problems: Compression of the optic nerves or optic chiasm, often causing loss of peripheral vision.
- Hormone Imbalances: Caused by the tumor either overproducing or underproducing certain pituitary hormones.
- Headaches: Severe or persistent headaches related to the tumor's size.
The Procedure Steps (Simplified)
The surgery is typically done under general anesthesia and often takes a few hours.
- Access (Nasal Phase): The ENT surgeon inserts the endoscope into one or both nostrils and navigates through the nasal cavity to the back wall of the nose.
- Corridor Creation (Sphenoidal Phase): The surgeon opens the front wall of the sphenoid sinus (an air-filled cavity behind the nose).
- Tumor Exposure (Sellar Phase): A small opening is made in the bone covering the pituitary gland, called the sella turcica. The dura (the membrane covering the brain) is opened.
- Tumor Removal: The neurosurgeon uses specialized, long instruments to remove the pituitary tumor in small pieces while visualizing the area on the monitor.
- Closure/Reconstruction: Once the tumor is removed, the surgical site in the sella is often reconstructed using tissue or grafts (sometimes from the nasal septum or abdomen) and biological glue to prevent a cerebrospinal fluid (CSF) leak. The instruments and endoscope are then removed.
After the Procedure
Recovery and Risks
Recovery Timeline
- Hospital Stay: Typically 2 to 3 days.
- Initial Recovery (First Weeks): You may experience nasal congestion, minor bloody drainage, headache, and fatigue. You must avoid blowing your nose, heavy lifting, or bending for several weeks.
- Return to Work/Activity: Many patients with sedentary jobs return in 2 to 4 weeks, with full recovery taking 4 to 6 weeks or more.
Key Risks
While minimally invasive, all surgery carries risks. Specific risks related to this procedure include:
- Cerebrospinal Fluid (CSF) Leak: Leakage of the fluid surrounding the brain, requiring immediate attention and potentially another surgery to repair.
- Hormone Imbalance: Damage to the normal pituitary gland tissue may necessitate lifelong hormone replacement therapy.
- Vision Damage: Though rare, damage to the optic nerve.
- Infection: Such as meningitis.
Benefits of endoscopic endonasal approach
- Minimally invasive
- Faster recovery time
- Reduced pain
- Lower risk of neurological damage
- Improved visualization
- Improved quality of life